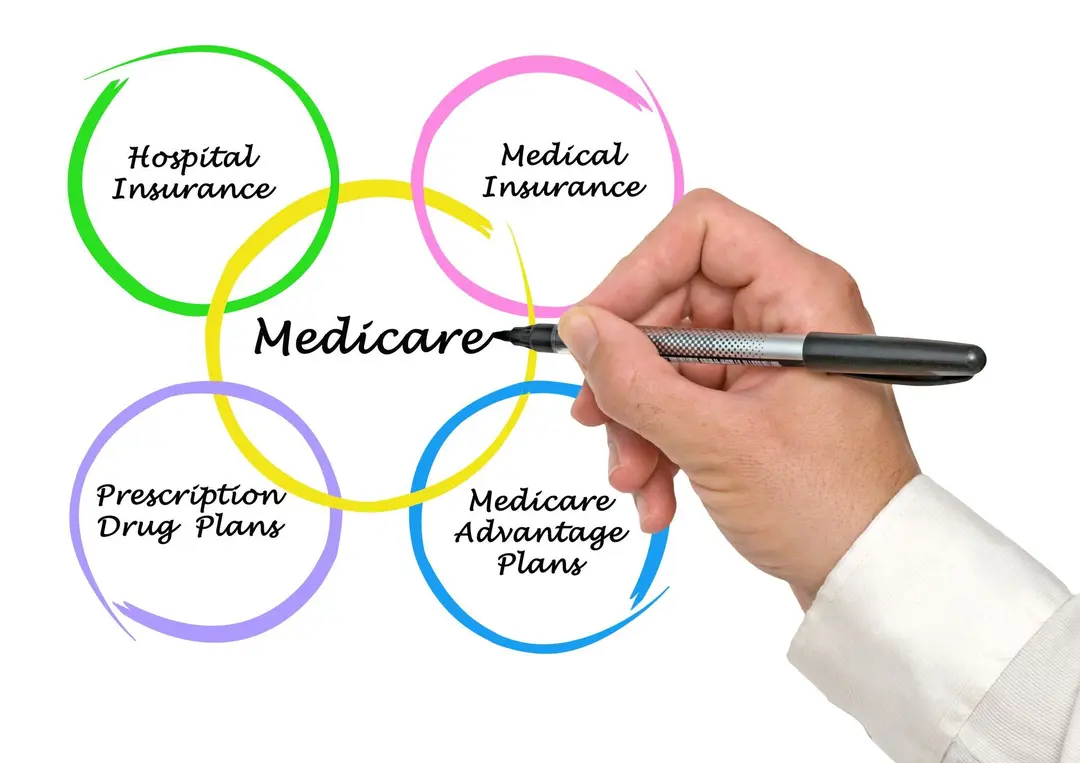
There are four different Medicare “Parts,” each of which offers different types of coverage. Medicare Part D only covers prescription medications and is typically purchased by itself in a standalone policy or rolled into a Medicare Advantage plan (Part C) for retirees who sign up for the added coverage. If you’re like many retirees, you may be wondering:
- What is not covered by Original Medicare (Part A and B)?
- \What is not covered by Medicare Part C?
What Is Not Covered by Original Medicare?
Original Medicare does cover a variety of medical services and supplies, but it’s more restrictive than many employer-provided health insurance plans and Medicare Advantage plans (Medicare Part C).
Original Medicare does not cover:
- Long-term care in assisted living communities or long-term custodial care
- Dental, vision or hearing care
- Cosmetic surgeries or elective procedures
- Podiatry (foot care)
- Acupuncture, massages or other alternative medicine and wellness services
- Health care overseas
- Prescription drugs
- Private nursing or home health aides
There are some scenarios in which some emergency services or necessary procedures of the above could be covered by Original Medicare. For example, if your doctors determine cataract surgery is medically necessary, it could be covered by Medicare Part B – even though vision care typically isn’t covered.
Even when some of these services are deemed medically necessary and covered, the services, treatments or medical devices to which the beneficiary is entitled will be inherently restrictive.
In other words, someone on Medicare Part B who did get their cataract surgery covered might not be entitled to the premium intraocular lenses that would correct their vision at multiple distances. If they did want the better lenses, they would have to pay the difference out of pocket.
While not all Medicare Advantage plans are equal, someone who does have Medicare Part C may be entitled to a variety of routine vision services, treatments and potentially even the premium lenses at no additional out-of-pocket cost.
What Is Not Covered by Medicare Part C?
- Long-term care, including nursing homes, assisted living and at-home care
- Any type of cosmetic surgery or elective surgery
- At-home assistance with activities of daily living (bathing, dressing, eating etc.)
- Experimental procedures and treatments
- High-cost dental procedures like dental implants
- Specialty prescription drugs
- Advanced or premium hearing aids
What is and isn’t covered by a Medicare Advantage plan is often dependent on the unique plan. Higher-cost plans may cover a wide range of procedures.
Coverage for Assisted Living, Nursing Care and Memory Care
There’s a notable absence in the coverage provided by Original Medicare and Medicare Part C – coverage for long-term assisted living, nursing care and memory care. An estimated 2 percent of U.S. seniors are currently living in assisted living facilities, with another 4 percent living in nursing homes. Both are pricey, with the average cost of assisted living being roughly $4,300 a month and the median cost of a private room in a nursing home being $9,000 a month. For comparison, the average cost for a full-time home health aide is just over $4,500 a month.
Medicare will cover some stays in skilled nursing facilities, inpatient hospital stays and hospice care, but the percentage covered varies based on the length of the stay. Luckily, there are alternative insurance options to cover or defray the cost of assisted living, memory care and nursing care.
Long-term care insurance is designed to cover costs associated with assisted living facilities, nursing homes, in-home care and other long-term care needs. The percentage of costs and the length of stay covered varies depending on the policy.
In other words, the higher the premium you pay, the longer the stay in assisted living or a nursing home will be covered – but these policies are typically finite. There’s also no renewing long-term care insurance, meaning if you had coverage for three years and use it up, you typically can’t renew the policy for another three years.
There are a variety of other financial tools retirees can potentially utilize to cover the cost of nursing care or assisted living, including certain veterans’ benefits and life insurance policies. Homeowners may also be able to leverage financing tools like a reverse mortgage to obtain funds for assisted living.
Retirees who exhaust all their insurance and assets may also qualify for Medicaid, which can defray many of the costs of long-term stays in some facilities.
Protect Yourself and Your Family From Ongoing Care Expenses
The most expensive part of retirement often comes at the end when the retiree requires full-time care and assistance in some type of nursing or memory care facility. Even people who saved for retirement may find their nest egg dwindling rapidly in a facility that costs $9,000 a month or more.
There are steps you can take as you near retirement age or even while you’re in retirement to safeguard yourself, your spouse and your family from these high costs. The team at Fullerton Financial Planning can explain your various insurance and financial options to ensure you don’t run out of resources or drain the assets you were hoping to pass on to your children or grandchildren. Call us at (623) 974-0300 to learn more.